Physiotherapy For Osteoarthritis 2023 is going to explain possible physiotherapy management of OA. before going to discuss Physiotherapy For Osteoarthritis lets have a look on osteoarthritis
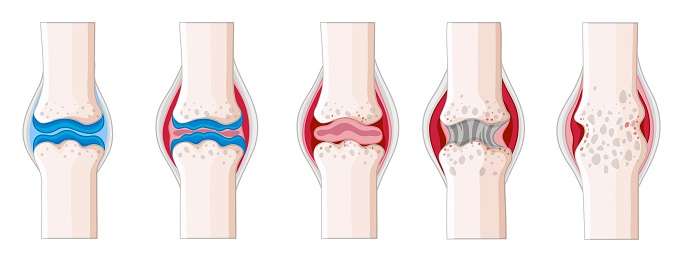
Osteoarthritis (OA) is a common joint condition affecting millions worldwide. It is a kind of arthritis that develops when the cartilage, which is the tissue that cushions the ends of bones in a joint, breaks down over time. As the cartilage gets tears, the bones may glides against each other, produces pain, stiffness, and inflammation. It causes bone spurs, or bony projections, around the affected joint.
Risk factors for developing OA include age, increased weight, joint repetitive stress, and certain medical conditions, such as diabetes and rheumatoid arthritis. Symptoms of OA can vary in severity, but they often include pain, stiffness, swelling, and restricted ROM.
Although there is no cure for OA, treatment can help manage the symptoms and improve joint function. Treatment options may include medication, exercise, weight management, physical therapy, and surgery.
Read more: Read more about Grades of Osteoarthritis
Table of Contents
Signs and Symptoms
Some common signs and symptoms of OA include:

Joint pain: Pain is one of the most common symptoms of OA. The pain is often described as a deep ache or a burning sensation, and it may be worse with activity or after prolonged periods of inactivity.
Stiffness: Joint stiffness is another common symptom of OA. The affected joint may feel stiff, particularly in the morning or after sitting for a prolonged period.
Swelling: In some cases, the affected joint may be swollen, tender to the touch, and warm to the touch.
Cracking or popping sounds: You may hear cracking or popping sounds when you move the affected joint. This is caused by the bones rubbing against each other due to the loss of cartilage.
Limited range of motion: As the joint deteriorates, you may experience a decreased range of motion, making it difficult to move the affected joint.
Changes in joint shape: Over time, the affected joint may change shape due to the development of bone spurs.
Weakness: You may experience weakness in the affected joint or the surrounding muscles.
If you are experiencing any of these symptoms, SEEK A healthcare professional, such as a rheumatologist or physiotherapist.
Causes of Osteoarthritis
The exact causes of osteoarthritis (OA) are not yet fully understood, but it is believed to be a complex condition caused by a combination of genetic, environmental, and lifestyle factors. Here are some of the factors that may contribute to the development of OA:
Age: OA is more common in older adults, as the cartilage in the joints tends to wear down over time.
Obesity: Being overweight or obese can put extra stress on the joints, particularly the knees and hips, increasing the risk of OA.
Joint injuries: A history of common injuries, such as fractures, dislocations, and ligament tears, can increase the risk of developing OA in the affected joint.
Genetics: Certain genetic factors may predispose individuals to develop OA, although the specific genes are not fully understood.
Joint misalignment: Abnormal joint alignment or mechanics can increase stress on certain joint parts, possibly increasing the risk of OA.
Repetitive stress: Repeated stress on a joint, such as that experienced by athletes or individuals with physically demanding jobs.
Associated diseases: diabetes, RA etc.
It’s important to note that while these factors may increase the risk of developing OA, not everyone at risk will develop the condition. Additionally, many people with OA have no identifiable risk factors. If you are experiencing joint pain or stiffness, seeing a healthcare professional, such as a rheumatologist or physiotherapist, is vital for an accurate diagnosis and appropriate treatment.
Diagnosis of Osteoarthritis
OA can be diagnosed by following means:
Medical history: Your Doctor will ask you about your symptoms, such as joint pain, stiffness, and swelling, as well as any past injuries or surgeries that may have affected your joints.
Physical examination: Your healthcare provider will perform a physical exam, looking for signs of joint swelling, tenderness, and limited ROM.
Imaging tests: CT Scan, MRI, and X-rays can help confirm the diagnosis of OA by showing the extent of joint damage and the presence of bone spurs or other signs of joint degeneration.
Laboratory tests: While there is no specific blood test for OA, your healthcare provider may order blood tests to differentiate it from other medical diseases such as RA
Physiotherapy For Osteoarthritis 2023
Physiotherapy For Osteoarthritis can be an effective treatment option for osteoarthritis (OA), a degenerative joint disease that causes joint pain and stiffness. Here in this article [Physiotherapy For Osteoarthritis 2023] some ways which can help manage the symptoms of OA:
Exercise: Physiotherapists can create an exercise program tailored to your needs and abilities. Exercise can help improve joint mobility, flexibility, strength, and balance, which can all help to reduce the pain and disability associated with OA.
Manual therapy may include joint mobilization and soft tissue techniques that can help reduce pain and stiffness in the affected joint.
Modalities: Certain modalities like ultrasound, heat or cold therapy, electrical stimulation or laser therapy can manage pain and inflammation associated with OA.
Education and self-management strategies: Physiotherapists can provide education about joint protection, activity modification, and assistive devices that can help reduce the impact of OA on daily activities and improve quality of life.
Overall, physiotherapy can have an essential part in the management of OA by enhancing joint function, reducing pain and stiffness, and improving overall physical function and quality of life. However, working with a physiotherapist with experience working with OA is essential to ensure that the treatment plan is appropriate and effective for your individual needs.
Exercises for Osteoarthritis
When it comes to osteoarthritis (OA) exercises, it is important to choose activities that can help maintain joint mobility, flexibility, and strength without causing pain or worsening the condition. Here are some exercises that can be helpful for people with OA:
ROM exercises: These exercises help to gain joint play and reduces hardness[stiffness] of joints. Examples include neck rotations, shoulder rolls, hip circles, and ankle rotations.
Strengthening exercises: These exercises can help improve muscle strength, reducing stress on the joints. Examples include wall squats, leg curls, and calf raises.
Low-impact aerobic exercises: These exercises can help to improve cardiovascular fitness without putting stress on the joints. Examples include walking, swimming, cycling, and water aerobics.
Balance exercises: These exercises can help to improve balance and prevent falls. Examples include standing on one leg, heel-to-toe walking, and tai chi.
It is essential to start slowly and gradually increase the intensity of the exercises over time.
Manual Therapy for Knee Osteoarthritis
Manual therapy can effectively treat knee osteoarthritis (OA), a degenerative joint disease that causes joint pain and stiffness. Here are some manual therapy techniques that may be used to manage the symptoms of knee OA:

Joint mobilization: This hands-on technique involves gently moving the knee joint in specific directions to help improve joint mobility and reduce pain.
Soft tissue techniques manipulate the soft tissues around the knee joint, including the muscles, tendons, and ligaments. Examples include massage, myofascial release, and stretching.
Taping involves using special tape to support the knee joint and lessen pain and inflammation.
However, working with a qualified and experienced manual therapist is essential to ensure that the treatment plan is appropriate and effective for your needs. Combining manual therapy with other treatments, such as exercise and medication, is vital to achieving the best possible outcomes.
Physiotherapy Modalities for Osteoarthritis
Several physiotherapy modalities can be used to manage the symptoms of osteoarthritis (OA). Here are some common modalities used in physiotherapy for OA:
Heat therapy involves applying heat to the affected joint to help improve blood flow, reduce pain and stiffness, and improve joint mobility. Examples include hot packs, warm water therapy, and infrared lamps.
Cold therapy involves applying cold to the affected joint to help reduce inflammation and pain. Examples include ice packs, cold water therapy, and ice massage.
Ultrasound therapy involves using sound waves to stimulate deep tissues and improve blood flow, which can help reduce pain and inflammation and promote tissue healing.
Electrical stimulation: This involves using electrical impulses to stimulate the affected muscles, which can help reduce pain, improve joint mobility, and promote tissue healing. TENS, NMES.
Laser therapy: This involves using light energy to stimulate the affected tissues, which can help reduce pain and inflammation, improve joint mobility, and promote tissue healing.
Working with a physiotherapist with experience using these modalities is vital to ensure that the treatment plan is appropriate and effective for your needs. Modalities are often combined with other treatments, such as exercise and manual therapy, to achieve the best possible outcomes.
Education and Self-management for Osteoarthritis
Education and self-management are essential components of treating osteoarthritis (OA). Here are some self-management strategies and education that can help manage the symptoms of OA:
Joint protection involves using techniques to reduce stress on the affected joint, such as avoiding activities that exacerbate pain or using assistive devices like knee braces or canes.
Weight management: weight is a major contributor of arthritic pain. managing weight help in the protection of joint from further damage.
Exercise: Exercise on daily basis is very beneficial in the management of OA.
Pain management: Several pain management strategies can be used to manage the pain associated with OA, including heat and cold therapy, medication, and relaxation techniques.
Nutritional support: Certain nutrients, such as vitamin D and calcium, are essential for maintaining bone integrity, which can help prevent progression of OA.
Emotional support: Living with a chronic condition like OA can be challenging. Emotional support from family, friends, and support groups can help manage the emotional impact of OA and improve the overall quality of life.
Overall, education and self-management strategies are essential components of the treatment of OA. Working with a healthcare professional, such as a physiotherapist or rheumatologist, can help you develop a comprehensive self-management plan that is appropriate and effective for your individual needs.
Physiotherapy Management of Osteoarthritis of the Knee
The management of osteoarthritis (OA) of the knee often involves a multidisciplinary approach, including physiotherapy. Here are some of the physiotherapy interventions that may be used in the management of knee OA:
Exercise: Regular exercise is an essential component of managing knee OA, as it can help improve joint mobility, strength, and function. Physiotherapists can design individualized exercise programs that include stretching, range of motion, and strengthening exercises, such as squats and lunges.
Manual therapy: Manual therapy involves the joint mobilizations and joint play, which reduce the chances of bony spur formation.
Modalities: heating modalities, laser therapy, cold therapy and TENS are most commonly using machines for the management of knee OA.
Assistive devices: Using assistive devices, such as knee braces or orthotics, may help support the knee joint and improve overall function.
Patient education: Education on proper joint mechanics, weight management, and self-management strategies, such as activity modification and pain management techniques, can help improve outcomes in knee OA.
Functional training: Functional training, such as gait training and balance exercises, can help improve overall mobility and reduce the risk of falls in individuals with knee OA.
It is important to note that the management of knee OA may vary depending on the severity of the condition and individual patient factors.
Physiotherapy Exercises for Knee Osteoarthritis
Here are some examples of physiotherapy exercises that may be recommended for individuals with knee osteoarthritis (OA):
ROM exercises: ROM exercises increases knee flexibility and mobility. These may include ankle pumps, knee extensions and flexions, and heel slides.
Strengthening exercises: can help improve knee joint stability and reduce pain. Examples of activities that can help support the knee include leg presses, squats, lunges, and step-ups.
Low-impact aerobic exercises: Low-impact aerobic exercises, such as walking, cycling, or swimming, can help better cardiovascular health and lessen pain and hardness in the knee joint.
Balance exercises: Balance exercises enhances stability and lowers the risk of falls in individuals with knee OA. Examples of balance exercises may include standing on one leg or using a balance board.
Proprioceptive exercises: Proprioceptive exercises can help improve joint position sense and neuromuscular control, which can help reduce the risk of further joint damage. Examples of proprioceptive exercises may include balancing on an unstable surface or using a wobble board.
Stretching exercises: stretches that may benefit knee OA include hamstring and quadriceps stretches.
A physiotherapist can design an individualized exercise program that addresses each patient’s specific needs. Additionally, it’s essential to follow any exercise program under the guidance of a healthcare professional.
